Cardiac Care
Cardiac Arrest
Symptoms
When to see a Doctor
Causes
Risk factors
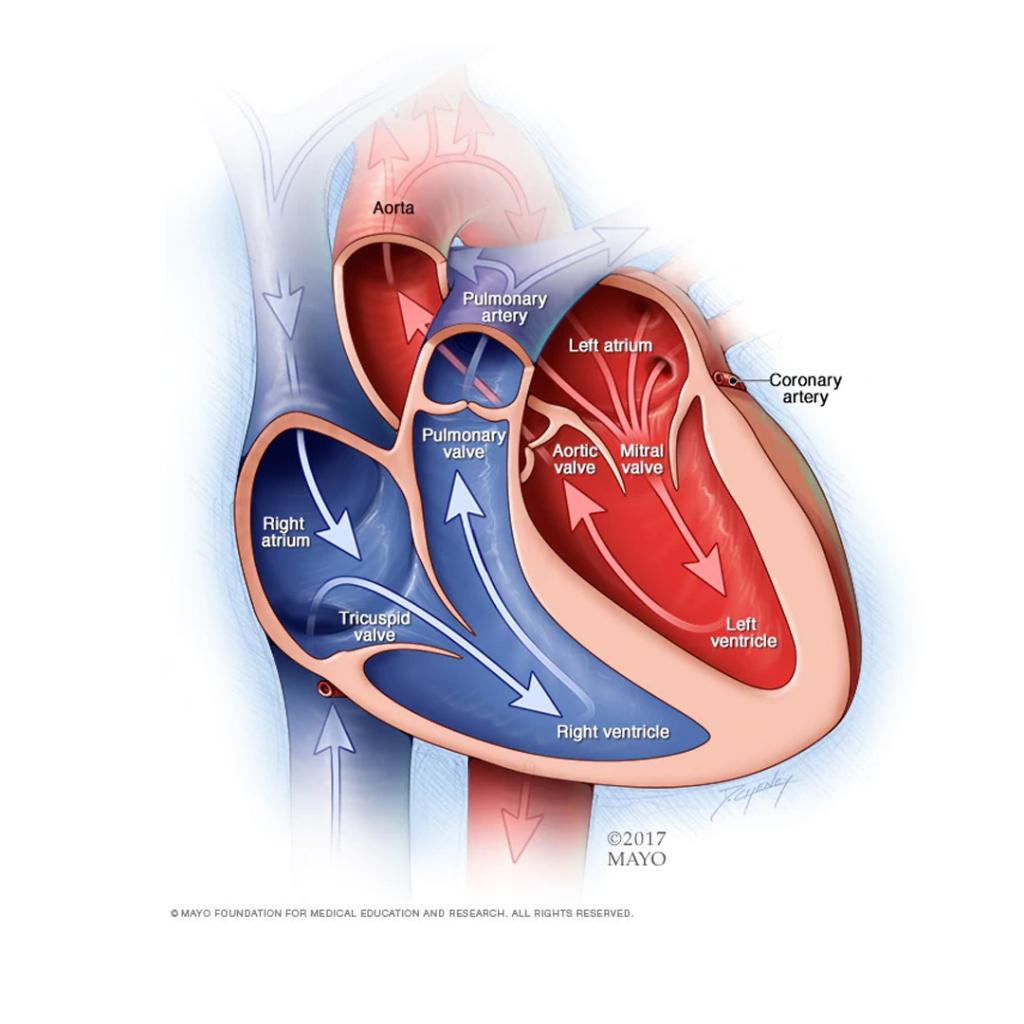
Chambers and valves of the heart
Because sudden cardiac arrest is so often linked with coronary artery disease, the same factors that put you at risk of coronary artery disease can also put you at risk of sudden cardiac arrest.
These include:
- A family history of coronary artery disease
- Smoking
- High blood pressure
- High blood cholesterol
- Obesity
- Diabetes
- A sedentary lifestyle
